NON-FUNCTIONING TUMORS

Non-functioning Tumors Definition
TUMORS ARE DIVIDED INTO FUNCTIONING & NON-FUNCTIONING
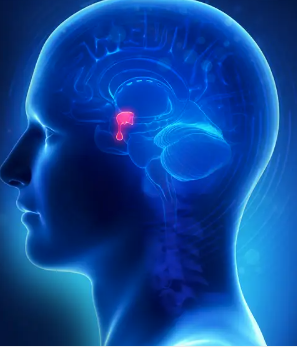
Pituitary tumors are commonly divided into "functioning" tumors (those that secrete pituitary hormones and cause clinical syndromes) and "non-functioning" tumors (those that do not secrete a pituitary hormone that leads to a clinical syndrome).
The functioning tumors make growth hormone and cause gigantism (in children) or acromegaly (in adults), make adrenocorticotropic hormone (ACTH) and cause Cushing's Disease, make prolactin and cause reproductive disturbances and breast secretion of milk, or very rarely make thyroid stimulating hormone (TSH) and cause hyperthyroidism. Therefore, tumors that do not make growth hormone, ACTH, prolactin, or TSH are non-functioning pituitary tumors. Approximately 30% of pituitary tumors are considered non-functioning. Non-functioning pituitary tumors, like all pituitary tumors, are virtually always benign, not malignant. These tumors are usually large when they are identified. Because they are non-functioning, they usually are not detected until they are large enough to cause the problems listed below. In retrospect, these tumors may have been causing symptoms for 5 to 10 years before detection.
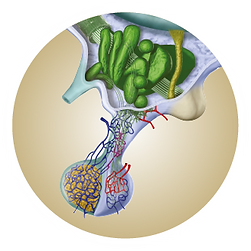
Careful studies of non-functioning pituitary tumors reveal that most actually do produce pituitary hormones. The most common hormone produced is follicle-stimulating hormone, or FSH. Other hormones that can be made by "non-functioning" tumors include luteinizing hormone (LH) and the alpha subunit of FSH and LH. Production of these hormones by "non-functioning" pituitary tumors can be documented in the patient by careful measurement of the hormones during various stimulation tests or by showing that the hormones are present in tissue removed at surgery by various laboratory techniques. In most cases, these tests are research tools and are not clinically indicated since they do not change the treatment of the tumor.
There are a number of reasons why these tumors appear non-functioning, even though they usually make at least one of the pituitary hormones. The first reason is that FSH and LH excess, unlike the pituitary hormones listed in the first paragraph, do not usually cause any specific symptoms. The second reason is that often only parts ("subunits") of the hormone are produced, and the subunits are not active. The third reason is that the hormones are often only secreted into the blood in small amounts, and therefore, blood levels are often normal. In premenopausal women, these tumors may cause ovarian cysts and menstrual abnormalities.

Clinical Presentation
THERE ARE THREE COMPONENTS TO ADULT GH DEFICIENCY
Patients with non-functioning pituitary tumors present with symptoms due to the size and location of the tumor, symptoms due to deficiency of pituitary hormones, or a combination of these two effects:
Symptoms are due to the size and location of the tumor. Any pituitary tumor (or any other tumor or other disease affecting the pituitary region) can cause headaches. Headaches may vary from mild to severe, and the severity is not always proportional to the size of the tumor. The headaches may be localized behind the eyes or be more generalized and can be mistaken for other types of headaches, such as tension or migraine headaches. Since these tumors are usually slow-growing and often become quite large before they are discovered, the headaches are often present for many years.
Another common symptom due to the size and location of the tumor is decreased vision. This tends to be a decrease in peripheral vision (termed "temporal visual field defects"), although other types of visual loss may also occur. This is due to the tumor growing upward and pressing on the optic chiasm, a nerve that carries visual information from the eyes to the brain. The decrease in peripheral vision may be quite extensive without the patient realizing it since people tend to rely on central, rather than peripheral, vision for most daily activities. Other less common vision problems due to pituitary tumors include double vision when looking up, down, or to the side. This is due to the tumor growing outward to the side and pressing on the nerves that control eye muscle movement.
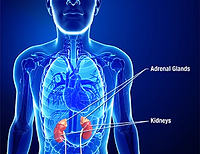
Symptoms are due to the loss of normal pituitary hormones. As non-functioning pituitary tumors grow, they compress the pituitary gland and interfere with normal pituitary hormone production. This can lead to deficiencies in the hormones that control sexual and reproductive function, the thyroid gland, the adrenal glands, and (rarely) water balance. Deficiencies of these hormones cause specific symptoms that are described in a separate section (see "hypopituitarism").
One pituitary hormone that can be increased, rather than decreased, by non-functioning tumors is prolactin. It is not unusual to see mild to moderate elevations in blood prolactin levels (up to 200 ng/ml) (normal 5-20 ng/ml) in patients with large non-functioning pituitary tumors. The source of the prolactin, in this case, is not the tumor but normal pituitary tissue that increases its prolactin production when the inhibitory effects of the brain are interrupted by the growing tumor. This can cause confusion among care providers who are not experienced in the evaluation of patients with pituitary tumors. A patient with a large, non-functioning tumor and a mildly elevated prolactin level can be misdiagnosed as having a prolactin-secreting pituitary tumor. This is an important mistake because prolactin-secreting tumors are treated with medication rather than surgery. The medication used for prolactin-secreting tumors will also lower blood prolactin levels in patients with non-functioning tumors, but the medication will not treat the tumor itself. In that case, the tumor may continue to grow while the patient and care provider are falsely reassured by the lower prolactin levels in the blood. For this, as well as other reasons, it is recommended that patients with large pituitary tumors be evaluated by endocrinologists experienced in pituitary tumors.

Clinical Evaluation
THERE ARE THREE COMPONENTS TO ADULT GH DEFICIENCY
Patients suspected of having a non-functioning pituitary tumor should have a high-resolution magnetic resonance imaging (MRI) study of the pituitary gland. An MRI provides the best visualization of the tumor size, location, extent, and relationship to important surrounding structures and is essential to adequately plan surgery and monitor treatment.
If the tumor seen on MRI is next to or distorts the optic chiasm, a formal assessment of vision should be performed by an ophthalmologist. This includes visual field measurements to assess damage to the optic chiasm and careful inspection of the optic discs. Visual field measurements can also be helpful in the follow-up of these tumors since they can be more sensitive to minor changes in tumor size than MRI.
In addition to the above tests done to assess tumor anatomy, patients with pituitary tumors should be evaluated for pituitary hormone deficiency by an experienced endocrinologist. The types of laboratory tests done for this evaluation will depend on the specific clinical findings, tumor characteristics, and treatment plans. The evaluation usually includes a measure of thyroid function, reproductive hormones, adrenal function, and growth hormone.

Treatment
THERE ARE THREE COMPONENTS TO ADULT GH DEFICIENCY
There are four treatment options for non-functioning pituitary tumors: observation, neurosurgery, radiation therapy, and medical therapy.
Observation
Observation without specific treatment can sometimes be appropriate for patients with non-functioning pituitary tumors, but this decision must be made carefully, and the patient must be closely followed. Observation is sometimes appropriate for smaller tumors that do not threaten vision or cause headaches or other symptoms. Most of these tumors are very slow-growing, and tumors that are not causing any problems can sometimes safely be watched. Observation may also be appropriate in older patients, even with large tumors, who have other serious medical problems and do not have a long life expectancy since the slow-growing tumor may not cause any problems in the patient's lifetime. In most cases, however, these tumors should be treated. Hormone replacement therapy may be indicated based on the results of the hormone-testing procedures.
Neurosurgery
In almost all cases, neurosurgery is the initial treatment of choice for nonfunctioning pituitary tumors. The surgery is usually performed through the nose ("transsphenoidal surgery"), which avoids having to dissect through the brain to reach the pituitary gland. The transsphenoidal route is appropriate even for very large tumors since these tumors can usually be adequately debulked via this route and since these tumors are rarely completely cured, even with more aggressive transcranial surgery. The goal in most cases of large tumors is to debulk the tumor rather than attempt to completely remove it. In the case of smaller tumors, a complete cure may be a reasonable goal.
The single most important factor in achieving optimal surgical results with large pituitary tumors (good debulking, few or no side effects, no damage to the normal pituitary gland and other normal structures) is an experienced surgeon with a good track record. Transsphenoidal surgery is best done by surgeons who perform many such operations every year and have documented good results with low rates of complications.
Radiation Therapy
Pituitary tumors are rarely treated primarily with radiation therapy since radiation therapy takes many years to be effective and usually leads to pituitary hormone deficiencies. However, in some cases, primary radiation therapy may be considered for these tumors. Newer methods for delivering radiation therapy to the pituitary gland (for example, the "gamma knife") appear to give more rapid results than traditional radiation therapy, though their effectiveness in controlling tumor growth is not necessarily greater.
Since many non-functioning pituitary tumors are large and cannot be completely removed by surgery, the issue of postoperative radiation therapy often arises. In many cases, the tumor has been sufficiently debulked and can be monitored without further treatment, even with a known residual tumor present. In other cases, postoperative radiation therapy is recommended. This decision is based on patient characteristics, as well as the size, location, and expected aggressiveness of the residual tumor.
Medical Therapy
Medical therapy has become important for the treatment of some functioning pituitary tumors, primarily prolactin and growth hormone-secreting tumors. Unfortunately, no clearly effective medical therapy for nonfunctioning pituitary tumors is currently available. In some, but not all, patients in whom surgery has been only partially successful or is contraindicated, dopamine agonists (cabergoline) or somatostatin analogs (octreotide) have been effective in suppressing tumor growth. However, these drugs should not be used as primary therapy. At the present time, the best treatment option for non-functioning pituitary tumors remains neurosurgical, while medical therapy awaits the development of more specific and effective drugs.