ACROMEGALY MENU
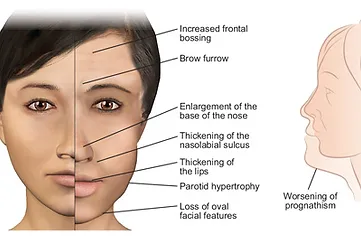
Changes in Facial Features in Acromegaly
Acromegaly
WHAT IS ACROMEGALY?
Acromegaly is a very rare disorder caused, in most cases, by a tumor of the pituitary gland that produces too much growth hormone (GH). Nearly all pituitary tumors, including those that cause acromegaly, are benign and not malignant. However, they can become quite large and expand beyond the normal confines of the pituitary gland. Rarely, acromegaly can be caused by a tumor located in other areas of the body.

Effects on Children & Adults?
HOW DOES ACROMEGALY AFFECT CHILDREN AND ADULTS?
Acromegaly can develop in people of any age but usually affects adults between the ages of 30 and 50. If acromegaly occurs in children, it causes gigantism, where the skeleton grows very quickly as an excessive amount of growth hormone is released by the pituitary tumor. Without treatment, the child grows very tall.
The structure of the bones of the arms and legs changes at around 17 or 18 years, when a person stops growing. This makes them unable to grow taller in adulthood. If acromegaly develops after a person has stopped growing normally, it does not affect their height. However, there are many other distinctive symptoms of acromegaly in both children and adults, and over the years, it can have serious health consequences such as diabetes, high blood pressure, and increased risk of heart disease and colon polyps.
Symptoms
WHAT ARE THE SYMPTOMS OF ACROMEGALY?
The development of symptoms in acromegaly varies from patient to patient. Symptoms tend to develop gradually, and the changes may not be noticed for years. Symptoms can develop due to both the increase in growth hormone levels and the physical presence of the growing tumor in the brain.
The effects of acromegaly can be very distressing and unpleasant, but most can be improved or reversed with treatment.
The abnormal growth hormone production leads to the overproduction of another substance, IGF-I, which stimulates the growth of bones and other tissues in the body. This can cause your hands, feet, and other parts of your body to enlarge. You may find that rings become tighter or need to be cut off, and shoe size may increase. Overgrowth of tissue in the hands can cause nerves to be compressed, resulting in tingling or pains in the hands - known as carpal tunnel syndrome. Your facial features may change, perhaps making the jaw and forehead more prominent and enlarging the lips, nose, and tongue. The skin may become thick and oily, and excessive sweating can be a problem. Headaches are also a common symptom.
As the tumor grows, it may cause headaches or impair peripheral vision as it presses on nearby nerves that run from the eyes to the brain. The tumor may damage the rest of the pituitary gland and cause underproduction of other hormones. The pituitary regulates many body processes, and damage to it in this way commonly results in problems with impotence, infertility, or irregular periods.
In addition to physical symptoms, acromegaly can be emotionally very traumatic. Symptoms such as loss of libido, exhaustion, and changing body image can be stressful, particularly as there may be some time before correct diagnosis and discussion of treatment. Even after this, anxiety about anticipated surgery so close to the brain and an understanding that recovery can take a while for some people can be difficult to cope with.

Diagnosis
WHAT ARE THE SYMPTOMS OF ACROMEGALY?
With acromegaly, you have higher than normal levels of growth hormone circulating in your blood due to continual overproduction by a tumor. To diagnose the condition, physicians must test your level of growth hormone. There are two ways this is commonly done.
IGF Test
Growth hormone secretion by the pituitary gland into the bloodstream leads to the production and release of insulin-like growth factor-one (IGF-I) from the liver and other tissues. If GH levels are high, IGF-I levels will also be high. Because IGF-I levels are much more stable over the course of a day than GH levels, this is often a more reliable test. The IGF-I test can be done with a single blood draw at any time of day and does not need to be a fasting sample. For these reasons, it has become the first test ordered to investigate excessive growth hormone secretion in many cases.
Glucose Tolerance Test
Growth hormone production fluctuates widely throughout the day but is normally suppressed after sugar-containing food or drink is eaten or drunk. For patients with acromegaly, sugar consumption will not reduce the high levels of the hormone as it does for patients without acromegaly. The glucose tolerance test is very reliable and is usually done in initial investigations of the condition. You will take a sugary drink, and the doctor will then take and test your blood for sugar and growth hormone at intervals over 2 hours.
Pituitary Function
If acromegaly is confirmed from the results of the tests above, the doctor will want to check that the non-tumor part of your pituitary gland is still functioning correctly. To do this, he or she tests your blood for other pituitary hormones. If some are low or missing altogether, they will be replaced with specific hormones - pills or injections that may need to be taken for the rest of your life.
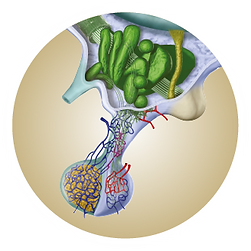
Scan
Next, the doctor will want to see exactly where and how big the pituitary tumor is. An MRI scan is used to do this. This type of brain scan is not painful. However, it requires the patient to lie in the tunnel-like scanner for about half an hour. A sedative can be provided if you are claustrophobic or anxious about it.
Treatment
TREATMENT OF ACROMEGALY
Acromegaly is treated very successfully in most cases. The aims of treatment are to reduce GH and IGF-I production to normal levels in order to reverse or improve the symptoms and to prevent or minimize damage to the rest of the pituitary gland and surrounding brain tissue by relieving the pressure exerted by the tumor.
Surgery to remove the pituitary tumor is often the preferred treatment, as it tends to give the best results in the shortest time. If an operation is not possible in your case, then drug treatment and/or radiotherapy may be used instead. Doctors often require a combination of treatments tailored to your needs and symptoms to get the very best results.
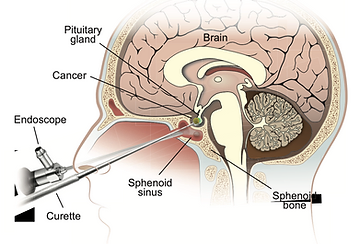
Surgery
The pituitary is located at the base of the brain, right in the middle of the skull. To reach it and remove a tumor, the surgeon makes a small incision at the back of the nose. This is called transsphenoidal surgery and, in most patients with acromegaly, avoids more invasive surgery. From here, the pituitary gland can be seen, and the surgeon uses special tools to remove the tumor tissue. The operation usually takes about an hour, and, in the best cases, the results can begin to be seen soon afterward. For example, facial features may begin to improve within a few days. Most often, the soft tissue changes are the first to noticeably improve. Sometimes, although GH levels have been reduced by the operation, the acromegaly is not cured. In these instances, you may be given additional treatment, such as drug therapy and/or radiotherapy.
Results depend on the size of the tumor and the skill of the surgeon. Removal of small tumors is generally more successful than large ones, and it is important to make sure that your surgeon is experienced in operating on the pituitary. If the tumor is completely removed and hormone levels return to normal, then surgery may be the only treatment for acromegaly you will need.
Drug Therapy
There are three different types of drugs currently used to treat acromegaly: ‘dopamine agonists,’ ‘somatostatin analogs,’ and ‘growth hormone receptor antagonists.’ Your doctor will advise on which is best for you, and this will be reviewed as treatment continues in case your condition is not improving or you are experiencing unpleasant side effects from one particular type.
Drug therapy may be chosen after surgery is determined to not completely improve your acromegaly, or in some cases, as an initial therapy without surgery.
Dopamine agonists such as bromocriptine (brand name Parlodel) and cabergoline (brand name Dostinex) inhibit GH release from the tumor. These drugs are the easiest to use as they are taken by mouth, especially cabergoline, which is taken just twice weekly, whereas bromocriptine must be taken two or three times daily. However, they are not always effective in treating acromegaly. Less than half of patients see a lowering of GH levels or reduction in tumor size with dopamine agonists. Additionally, side effects such as constipation and dizziness when standing can be experienced. If the drug is introduced slowly and dosage built up over time, these effects can usually be avoided.
Dopamine agonists are often thought of as first-line medical therapy. However, they are less effective than the other medications. However, dopamine agonists are easier to take and are less costly, so they may be used in some cases. However, other medications are more commonly used to treat acromegaly. If dopamine agonists are not working for you, your doctor may change your medication to ‘somatostatin analogs.’ Dopamine agonists and somatostatin analogs have the same aim: to stop the tumor from releasing growth hormone, but they act in different ways.
Two types of somatostatin analogs are available: octreotide (brand name Sandostatin) and lanreotide (brand name Somatuline). Octreotide comes in two forms, the first of which must be injected under the skin (subcutaneously) three times a day. Patients are given training to correctly inject themselves with this medication. The second form is longer-lasting (brand name Sandostatin LAR Depot) and is injected once a month deep into muscle (intramuscularly). A nurse usually performs the intramuscular injections.
Lanreotide is available as a deep subcutaneous injection (brand name Somatuline Depot) that is also long-lasting. Injections are usually given once a month but can be given less frequently to some patients. The injection can be given by a nurse or the patient’s partner. There is little difference in the effectiveness of these two somatostatin analogs. In addition to their effects on reducing GH and IGF-I levels, somatostatin analogs decrease the size of the tumor in most patients.
Somatostatin analogs can cause side effects on the stomach or digestive system. When you start the treatment, it may cause bloating or diarrhea, although this tends to wear off after a few days. In the long term, you may experience side effects such as gas or nausea, and octreotide may cause gallstones, although these rarely cause problems.
The third type of drug treatment is a growth hormone receptor antagonist, and the only drug in its class is called pegvisomant (brand name Somavert). Unlike dopamine agonists and somatostatin analogs, pegvisomant does not stop the production of GH by the tumor. Instead, it stops the hormone from taking effect in the body. Pegvisomant is taken in the form of a daily injection under the skin that patients can administer themselves. The drug is well-tolerated, though patients must be tested for liver abnormalities while on therapy. Also, pegvisomant does not improve headaches and does not reduce tumor size or growth.
Radiotherapy
If it is not possible for you to have an operation, or if some tumor tissue remains after surgery that is not responsive to drug therapy, radiotherapy (treatment with targeted radiation) might be needed. Please rest assured that even if you are offered radiotherapy for acromegaly, it does not mean that you have cancer. There are a variety of types of radiotherapy, but all work using the same principle. Depending on the type of radiotherapy, radiation beams carefully targeted at the tumor are given in small doses at a single time or daily over a month or so. Radiotherapy causes a gradual reduction in tumor size and GH release, so the improvement of the acromegaly is not as quick or as noticeable as with surgery. However, you may continue to see the results of radiotherapy over several years. Your doctor will monitor you for years after the radiation treatment because it is common for other pituitary functions to be affected by the radiation, and you may need pituitary hormone replacement therapy.
Drug treatment is usually given to reduce your GH and IGF-I levels while you wait to see the results from the radiotherapy.
Monitoring Treatment
A doctor carefully monitors the success of treatment for acromegaly in each individual patient. This is done by assessing the problems that acromegaly causes you and by measuring the relevant hormones. Your doctor will ask if there has been a change in hands, feet, or other areas and discuss changes in other symptoms that you might have noticed. Blood tests to measure GH and IGF-I levels will be taken several times each year. The aim of treatment is to lower your GH level to less than one ng/ml and to have your IGF-I level in the normal range for your age.
What You Can Expect from Treatment
If surgery isn’t an option, or if it is not successful, it may take a little time for your doctor to find the best treatment suited to you. However, once an appropriate therapy is found, you can expect to start seeing a significant improvement in your symptoms. With treatment such as radiotherapy, changes will be gradual and can take months or even years to give full results, whereas benefits from surgery and drug therapy are often seen within days or weeks.
Once treatment is successful, you can expect to notice that your hands and feet become less swollen and decrease in size – relieving any carpal tunnel syndrome – while facial features often return gradually to normal. If you were suffering from excess sweating, this should decrease, and if you had type 2 diabetes, it should improve or disappear altogether. Headaches usually improve, and eyesight usually returns to normal. Life expectancy is decreased in patients with acromegaly but is restored to normal with successful treatment.
Frequently Asked Questions
Patients with uncontrolled Acromegaly have an increased risk of dying earlier than expected. Lowering the excessive hormone level to normal reduces this risk. Complications associated with acromegaly that can affect your life span include heart failure, high blood pressure, abnormal cholesterol, diabetes, snoring and other sleep-related breathing problems, and joint disease.
Unfortunately, by the time most patients are diagnosed with acromegaly (usually a delay of many years after the beginning of symptoms), the pituitary tumor is large and may invade areas that the surgeon cannot easily access, or the tumor has invaded surrounding structures. The surgical remission rates depend on the size of the tumor and the expertise of the surgeon. Surgery is usually effective in removing the bulk of the tumor, relieving headaches, and improving visual problems, but it may not be possible to remove the entire tumor. Additional treatments are often necessary to lower serum GH and IGF-I levels to normal in order to reduce the risk of complications from continued excessive growth hormone production.
While the tumor makes growth hormone, its action and effect are dependent on the production of IGF-I (insulin-like growth factor-one). Blood IGF-I is produced primarily in the liver in response to the amount of GH made by the pituitary gland. The blood IGF-I level is a reliable indicator of overall growth hormone production. Since blood growth hormone levels fluctuate every few minutes over 24 hours, a single growth hormone level is only a “snapshot” in time and does not reflect overall growth hormone production. The blood IGF-I level is the most reliable indicator of overall growth hormone production. A normal blood IGF-I level usually indicates remission or, in patients taking medication, control of acromegaly.
Somatomedin-C is an older name for the same hormone, IGF-I.
Medical treatment is usually given if patients are not cured by surgery. In some cases, medical therapy may be used as the first line of therapy or for a few months before surgery. This depends on the size and location of the tumor. Although medications can lower growth hormone and/or IGF-I levels, they do not always shrink the tumor. Because of the long-term complications of excessive growth hormone (joint problems, diabetes, high blood pressure, facial changes, risk of colon polyps, premature heart disease, and premature death), it is important to reduce growth hormone and/or IGF-I to normal. Radiation therapy for the remaining tumor is another option. Since it may take several years before the radiation therapy is effective, medical treatment is used to control excessive growth hormone production while waiting for the effects of radiation. Medications do not cure the problem - they control it. The medication is effective only as long as it is taken as prescribed.
Currently, used drugs include:
- Dopamine Agonist: Cabergoline (Dostinex)
- Somatostatin Analogs: Octreotide (Sandostatin), octreotide LAR (Sandostatin LAR), lanreotide auto gel (Somatuline depot).
- Growth Hormone Receptor Antagonist: Pegvisomant (Somavert).
The dopamine agonist drug cabergoline may improve symptoms but is not very effective, resulting in normal hormone levels in less than 30%. In addition, patients more likely to respond are those in whom IGF-I and GH levels are only slightly elevated.
Octreotide-LAR and Lanreotide Autogel lower growth hormone and, therefore, IGF-I levels. They are given as an injection every 28 days or sometimes less frequently. They reduce growth hormone and IGF-I levels in approximately 90% of patients. However, lowering these hormone levels to normal occurs in approximately 45% to 60% of patients. Some patients have a better response to the combination of octreotide or lanreotide and cabergoline. In patients who still have mild elevations of IGF-I levels during octreotide or lanreotide treatment, the addition of cabergoline may reduce IGF-I levels to normal. Regardless of which regimen is used, these medications do not cure the disease; they control excessive growth hormone production by the tumor. Therefore, the medication(s) is effective only as long as it is taken regularly.
Pegvisomant (Somavert): This medication does not act on the pituitary tumor - it blocks the action of growth hormone at the liver and other sites to reduce the production of IGF-I. Approximately 80% of patients treated with Somavert have a reduction in IGF-I to normal. Because the medication doesn’t act on the tumor, the tumor itself is not treated. Although most tumors that secrete growth hormone grow slowly, there is a risk of continued growth of the tumor in Somavert-treated patients. This medication, therefore, is not typically used without other treatments if the tumor is large or showing signs of growth. Regular MRI scans are necessary to find out if there is growth of the pituitary tumor in patients treated with Somavert. This medication is given as an injection under the skin with a small needle similar to the needle used to give insulin for diabetes and is self-administered once a day. Sometimes, pegvisomant is administered less frequently (once or twice a week) or daily in lower doses in association with octreotide, lanreotide, or cabergoline when GH and IGF-I are not completely controlled by these medications alone.
Cabergoline: Occasional nausea, vomiting, dizziness (especially when standing up quickly). At much higher dosages (we used in patients with Parkinson’s disease), it may cause damage to the heart valves.
Octreotide, Lanreotide: When beginning treatment: loose stools, light-colored stools, occasional diarrhea, and abdominal cramping. This side effect usually lessens or disappears within 1 to 2 weeks. The long-term side effect is the risk of developing gallstones - approximately 25% of people develop gallstones or gall bladder sludge, as seen on ultrasound testing. The gallstones usually do not cause a problem and, in most patients, do not cause symptoms. However, there is always a small risk of developing problems.
Pegvisomant (Somavert): Development of abnormal liver tests occurs in some patients, more frequently if they have diabetes and/or are co-treated with octreotide or lanreotide. The tests return to normal when the medication is stopped. Therefore, it is recommended that liver tests be measured before beginning treatment, every month for the first six months of pegvisomant treatment, and at regular intervals afterward. Growth of the remaining tumor has occurred in a few patients; this means that regular MRI studies are necessary to detect this. Previous radiation treatment to the tumor appears to make it less likely that there will be tumor growth, but regular MRI scans are necessary to make sure there is no growth.
Occasionally, but not usually. Most patients have a macroadenoma (tumor greater than 1 cm) at the time of diagnosis. In this situation, surgery to remove as much of the tumor as possible is usually the first treatment. This is particularly important if the tumor is close to the eye nerves (optic chiasm). If the patient cannot undergo surgery, or there is no clear benefit of surgery, medical treatment, preferably with, is used.
Approximately one-third of patients have a reduction in tumor size when treated with octreotide or lanreotide. The amount of tumor shrinkage is usually modest, approximately 30%. Pegvisomant (Somavert): No; this medication does not act directly on the growth hormone-producing tumor - it acts to block the action of growth hormone on the liver, reduces IGF-I production, and does not cause a reduction in tumor size.
Sandostatin LAR: The Novartis patient assistance telephone number is (877) LAR-HELP.
Somatuline Depot: The Ipsen patient assistance number is called PACE, and the number is (866) 435-5677.
Pegvisomant (Somavert): The Pfizer Bridge program telephone number is (800) 645-1280.