Hypopituitarism Menu

What is Hypopituitarism?
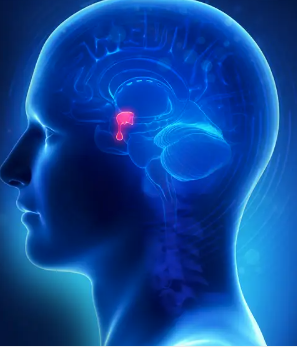
SMALL GLAND AT THE BASE OF THE BRAIN
The pituitary gland is a small gland attached to the base of the brain. Hypopituitarism refers to loss of pituitary gland hormone production. The pituitary gland produces a variety of different hormones:
- Adrenocorticotropic hormone (ACTH): controls production of the adrenal gland hormones coritsol and dehydroepiandrosterone (DHEA).
- Thyroid-stimulating hormone (TSH): controls thyroid hormone production from the thyroid gland.
- Luteinizing hormone (LH) and follicle-stimulating hormone (FSH): LH and FSH together control fertility in both sexes and the secretion of sex hormones (estrogen and progesterone from the ovaries in women and testosterone from the testes in men).
- Growth hormone (GH): required for growth in childhood and has effects on the entire body throughout life.
- Prolactin (PRL): required for breast feeding.
- Oxytocin: required during labor and delivery and for lactation and breast feeding.
- Antidiuretic hormone (also known as vasopressin):
Hypopituitarism may involve the loss of one, several or all of the pituitary hormones. Thus, a complete evaluation is needed to determine which hormone or hormones are deficient and need to be replaced. Hormone replacement is available for all of the pituitary hormones except for PRL and oxytocin. 'Hypo' is Greek for 'below normal' or 'deficient'.

What Causes Hypopituitarism?
MOST COMMON CAUSE IS A PITUITARY TUMOR
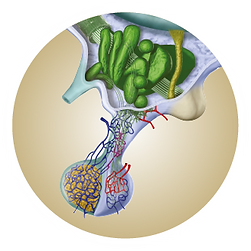
There are numerous causes of hypopituitarism (see Table 1). The most common cause of hypopituitarism is a pituitary tumor (also known as a pituitary adenoma). Pituitary adenomas are almost invariably benign (not cancerous). However, the pituitary adenoma itself may put pressure on the remaining normal part of the pituitary gland and limit or even destroy its ability to produce hormones appropriately.
The normal pituitary is compressed by the tumor which may cause hypopituitarism. (reprinted with permission, from Kronenberg H, Melmed S, Polonsky K, Larsen PR (eds): Williams Textbook of Endocrinology, 11th Edition, Chapter 8, Anterior Pituitary, Melmed S and Kleinberg DL authors, Philadelphia, Penn: WB Saunders; 2008.)
Sometimes pituitary adenomas produce too much of one hormone (e.g., GH or PRL), which is called hyperpituitarism, while simultaneously causing underproduction of other hormones produced in the adjacent normal pituitary gland. In this case, reduced levels of some hormones (e.g., hypopituitarism due to thyroid, adrenal, and sex hormone dysfunction) can be accompanied by overproduction of other hormones.
Hypopituitarism can also result from pituitary surgery, which might damage part of the normal pituitary. It can result from radiation treatment that, over time, also might damage the normal pituitary, even if the pituitary gland was working normally when the patient was first diagnosed with the pituitary adenoma. Therefore, a full pituitary hormone assessment is required both before and after surgery or radiation treatment.
Other tumors that grow near the pituitary gland (e.g., craniopharyngioma, Rathke’s cleft cyst) can cause hypopituitarism. In addition, tumors that metastasize from cancers elsewhere in the body can spread to the pituitary gland and can lead to hypopituitarism.
Inflammation of the pituitary can also cause hypopituitarism (see Table 1). Sarcoidosis and histiocytosis are types of chronic inflammation that also can result in hypopituitarism.
Radiation that focuses on a pituitary tumor or on the whole brain can result in loss of pituitary hormone production over time. In fact, it should be an expected consequence of radiation therapy. However, it may not occur for months or even years after the treatment. Thus, regular monitoring of pituitary hormone production is essential.
Pituitary apoplexy refers to a sudden hemorrhage into a pituitary adenoma and can cause rapid onset of pituitary insufficiency. This may cause double vision and/or visual loss, feeling quite ill, and may be an emergency requiring immediate attention.
Severe head trauma, usually accompanied by coma or other neurologic problems, can also cause hypopituitarism. Approximately 15% of patients with a history of severe head trauma have been found to be GH deficient. Other hormone deficiencies may also occur after severe head trauma.
TABLE 1. SIGNS AND SYMPTOMS OF CUSHING'S SYNDROME
| CAUSE | EXAMPLE |
|---|---|
| Pituitary Adenomas | Non-functioning pituitary adenoma Functioning pituitary adenoma Surgery on pituitary adenoma |
| Other Tumors Near the Pituitary | Craniopharyngioma Rathke’s pouch cysts Metastatic tumors |
| Radiation Treatment | To the pituitary To the brain |
| Inflammation | Hypophysitis Tuberculosis Meningitis Sarcoidosis Histiocytosis |
| Hemorrhage (Apoplexy) | Sheehan’s syndrome (associated with a hemorrhage during childbirth) |
| Severe Head Trama |

What Are the Symptoms of Hypopituitarism?
SYMPTOMS DEPEND ON WHICH HORMONE(S) ARE MISSING.
ACTH Deficiency Causing Cortisol Deficiency: Symptoms include weakness, fatigue, weight loss, abdominal pain, low blood pressure, and low serum sodium levels. During a period of severe stress, such as infection or surgery, cortisol deficiency may potentially result in coma and death. ACTH also stimulates DHEA secretion from the adrenal cortex.
TSH Deficiency Causing Thyroid Hormone Deficiency: Symptoms include fatigue, weakness, difficulty losing weight, generalized body puffiness, feeling cold, constipation, difficulty with memory, and an inability to concentrate. The skin may become dry and the complexion pale. In addition, anemia, high cholesterol levels, and liver problems may also occur. Patients with severe or long-term deficiency can appear lethargic. Rarely, severe thyroid hormone deficiency can cause coma, low body temperature, and even death.
LH and FSH deficiency in Women: LH and FSH deficiency may cause loss of menstrual cycles, infertility, decrease in sex drive and vaginal dryness, and osteoporosis, which can result in a tendency to develop bone fractures.
LH and FSH deficiency in Men:LH and FSH deficiency may cause loss of libido (interest in sexual activity), difficulty in achieving and sustaining an erection, infertility due to a low sperm count, and osteoporosis, which can result in a tendency to develop bone fractures.
GH Deficiency: In children, GH deficiency causes slowing or lack of growth and an increase in body fat. In adults, GH deficiency may cause a decrease in energy and physical activity, a change in body composition (increased fat, decreased muscle mass), a tendency toward increased cardiovascular risk factors/diseases, and a decreased quality of life (including an increased sense of social isolation).
PRL Deficiency: In the case of PRL deficiency, the mother might not be able to breastfeed following delivery.
Antidiuretic hormone deficiency: This hormone deficiency results in diabetes insipidus (DI). DI is not the same as diabetes mellitus, which is also known as type 1 or type 2 diabetes or sugar diabetes. Symptoms of DI include increased thirst and frequent urination, particularly at night. Pituitary adenomas themselves rarely cause DI unless it occurs after surgery. If DI occurs spontaneously, it usually indicates that some other sort of tumor or inflammation is present in the area.
Sexual desire in women is partially controlled by the hormone DHEA (which is controlled by ACTH). DHEA is a weak androgen (a male hormone like testosterone). In men, DHEA is of little functional relevance because much higher levels of the potent male hormone testosterone are present. However, in women, DHEA deficiency can contribute to impaired quality of life (tiredness, depression) and impaired sexual desire and enjoyment.
TABLE 2. SYMPTOMS AND SIGNS OF PITUITARY HORMONE DEFICIENCY
| PITUITARY HORMONE | TARGET ORGANS | TARGET ORGANS |
|---|---|---|
| ACTH | Adrenal glands: cortisol and DHEA | Fatigue, low sodium in blood, weight loss, skin pallor |
| Hypertension | Thyroid gland: thyroid hormone | Fatigue, weight gain, dry skin, sensitivity to cold, constipation |
| TSH | Ovaries: estrogen, progesterone; ovulation | Loss of periods, loss of sex drive, infertility |
| LH and FSH in Women | Testes, testosterone, sperm production | Loss of sex drive, erectile dysfunction, impotence, infertility |
| GH in Children & Adolescents | Bone, muscle, fat | Lack of growth (height); increased body fat, failure to achieve normal peak bone mass |
| GH in Adults | Whole body | Poor quality of life, increased body fat, decreased muscle and bone mass |
| PRL | Breast | Inability to breast feed |
| Oxytocin | Breast, Uterus | Complete deficiency could make breast feeding difficult |
| Antidiuretic Hormone (Vasopressin) | Kidney | Frequent urination (day & night), dilute urine, excessive thirst |

How is Hypopituitarism Diagnosed?
DIAGNOSED BASED ON THE PATIENT'S SYMPTOMS
Hormone deficiency is diagnosed based on the patient’s symptoms and the results of blood and sometimes urine tests. When a pituitary adenoma or other tumor is detected near the pituitary or when a person is exposed to some other potential cause of hypopituitarism, the patients should be evaluated for hypopituitarism.

What Tests are Necessary?
CAN DEVELOP IN PEOPLE OF ANY AGE
The tests needed to make a diagnosis depend on the patient’s symptoms, the type of pituitary problem, and the type of treatment received (surgery, radiation). In general, a patient with a large pituitary adenoma is more likely to have a hormone deficiency than a patient with a small adenoma. A single blood test to determine the pituitary and target organ hormone levels may be all that is needed.
Sometimes, a stimulation test is necessary to determine if there is a hormone deficiency. This is particularly true when evaluating cortisol or GH deficiencies. In the first kind of stimulation test, the patient is administered a hormone such as synthetic ACTH (“Synacthen test”), and then adrenal function is assessed. For a GH stimulation test, GH-releasing hormone (with an amino acid, arginine) is injected into the vein, and then GH levels are evaluated. A combined test to assess cortisol and GH deficiency involves giving the patient a small dose of intravenous insulin. Insulin causes a reduction in blood glucose, and the low glucose level itself increases both cortisol and GH levels. Stimulation tests must be conducted under careful medical supervision. Important: An insulin tolerance test should not be performed in elderly patients or patients with a history of heart disease, stroke, or epilepsy.
Thyroid hormone deficiency is diagnosed by measuring the levels of TSH (pituitary hormone) and thyroid hormone (produced by the thyroid) in the blood. The level of thyroid hormone itself is the more important measurement for making the diagnosis.
In women, a diagnosis of LH and FSH deficiency is determined based on the menstrual history. Regular menstrual cycles in women not taking oral contraceptives usually mean there is no deficiency. Women who are menopausal are expected to have elevated LH and FSH levels because their ovaries no longer work effectively; therefore, normal or low LH and FSH levels in menopausal women usually indicate a deficiency in one or both of these pituitary hormones.
In men, LH and FSH deficiencies are determined by asking about sex drive and ability to have erections and by measuring the LH, FSH, and testosterone levels in the blood. If the testosterone level is below normal and LH and FSH levels are normal or low, hypopituitarism regarding sex hormones is confirmed. These men might also have noticed a reduction in the size of the testes, which may also be soft. For men who are concerned about fertility, a semen analysis (measures number of sperm and quality of sperm movement) is necessary.
Antidiuretic hormone deficiency (diabetes insipidus) is suggested on the basis of symptoms of increased thirst and an increased amount and frequency of urination, particularly at night. A 24-hour urine collection may be used to confirm the output of large volumes of urine. Blood and urine tests are important for confirming the diagnosis. A high level of sodium in the blood and low urine concentrating ability indicate a diagnosis of DI. Occasionally, to confirm a diagnosis of DI, the patient is hospitalized so a water deprivation test can be performed. The test involves withholding fluid and measuring blood sodium and osmolality over several hours. The time it takes to conduct the test depends on the severity of the DI.

How is Hypopituitarism Treated?
TREATED BY REPLACING THE DEFICIENT HORMONES
Hormone deficiency is treated by replacing the deficient hormones. The goals of treatment are to improve symptoms (see Table 2) and to replace the deficient hormone or hormones at a level that is as close to physiologically correct (“mother nature”) as possible. However, one rule of hormone replacement is that no one dose will suit every patient.
Thus, when hormone replacement therapy is prescribed, the patient will need to be seen regularly after starting treatment to assess the effect. It often takes time and repeated dose changes to find the optimal dose for each patient. Typically, once the optimal dose is determined, the dose remains adequate for long-term treatment unless other medications are added or the patient’s condition changes in a way that alters the blood levels (e.g., introduction of GH therapy may require an increase in cortisol replacement, whereas pregnancy may require an increase in the dose of thyroid hormone).
Cortisol: On average, cortisol replacement therapy consists of giving approximately 15 mg of cortisol daily in divided doses. Approximately 2/3 of the dose is given in the morning and 1/3 in the late afternoon or evening. Excess cortisol can cause side effects (see the section on risks below), so it is best to use cortisol replacement in doses that are adequate but not too high.
Some endocrinologists prescribe prednisone instead of cortisol, and the dose of prednisone can be given once or twice a day. Patients with cortisol deficiency must always remember that during periods of stress, their bodies may not be able to produce the increased level of cortisol needed. Therefore, patients should always carry a medical or steroid alert card or wear a medical alert bracelet or necklace to inform physicians that they are taking chronic steroid therapy. If patients have multiple pituitary hormone deficiencies, cortisol should always be the first hormone replaced, as medications like thyroid hormone or GH can increase the body’s need for cortisol.
Thyroid Hormone: Levothyroxine is given daily as the therapy for thyroid hormone deficiency.
- Most people with hypothyroidism have disease directly in the thyroid gland and are said to have primary hypothyroidism. Patients with primary hypothyroidism have elevated levels of TSH and low levels of thyroid hormone. In this situation, treatment with thyroid hormone causes the level of thyroid hormone to increase and the level of TSH to decrease.
- Patients with hypothyroidism as a result of pituitary disease are said to have secondary hypothyroidism. Such patients have low levels of both TSH and thyroid hormone (see Figure 2). Although treatment with thyroid hormone should increase the level of thyroid hormone in the blood to the normal range, it would not change the level of TSH. Thus, TSH is not used to monitor dosing in patients with secondary hypothyroidism. Instead, the physician has to rely on signs and symptoms and measurement of thyroid hormone in blood.
Sex-Related Hormones: Women: Premenopausal women who have no menstrual cycles as a result of pituitary disease (secondary hypogonadism) should receive replacement therapy with estrogen and progesterone. Estrogen can be given orally, by patch, or by gel. Progesterone equivalent is only required in women who have an intact uterus. Women who have undergone a hysterectomy can be treated with estrogen alone.
Men: In testosterone-deficient men, testosterone is given by patch, gel, or injection either daily (patch or gel) or every 2–4 weeks by intramuscular injection.
GH Therapy: GH prescribing practices vary depending on local customs, national guidelines, and insurance coverage. It is important to do tests to prove that patients are indeed GH deficient. Human GH is administered by daily injection. Most pituitary endocrinologists start at relatively low doses to avoid side effects and increase as needed.
DI Therapy: Desmopressin is usually given in tablet or spray form (nasal tube or nasal spray). Hospitalized patients may be given desmopressin by injection.
TABLE 2. SYMPTOMS AND SIGNS OF PITUITARY HORMONE DEFICIENCY
| PITUITARY HORMONE | TARGET ORGANS | TARGET ORGANS |
|---|---|---|
| ACTH | Adrenal glands: cortisol and DHEA | Fatigue, low sodium in blood, weight loss, skin pallor |
| Hypertension | Thyroid gland: thyroid hormone | Fatigue, weight gain, dry skin, sensitivity to cold, constipation |
| TSH | Ovaries: estrogen, progesterone; ovulation | Loss of periods, loss of sex drive, infertility |
| LH and FSH in Women | Testes, testosterone, sperm production | Loss of sex drive, erectile dysfunction, impotence, infertility |
| GH in Children & Adolescents | Bone, muscle, fat | Lack of growth (height); increased body fat, failure to achieve normal peak bone mass |
| GH in Adults | Whole body | Poor quality of life, increased body fat, decreased muscle and bone mass |
| PRL | Breast | Inability to breastfeed |
| Oxytocin | Breast, Uterus | Complete deficiency could make breastfeeding difficult |
| Antidiuretic Hormone (Vasopressin) | Kidney | Frequent urination (day & night), dilute urine, excessive thirst |
TABLE 3. HORMONE REPLACEMENT OPTIONS
| DEFICIENT PITUITARY HORMONE | MEDICATION | HOW TAKEN |
|---|---|---|
| ACTH | Usually, hydrocortisone or prednisone | Tablets, once or twice a day, depending on which drug |
| TSH | Thyroid hormone - usually T4 (thyroxine) | Tablets daily |
| LH and FSH in Women | Estrogen, progesterone | Tablets, skin patches, gels |
| LH and FSH in Men | Testosterone | Gel or skin patch, every day; injection in the buttock or thigh, every 2-4 weeks |
| GH in Children & Adolescents | GH | Daily injection under the skin (very small needle) |
| GH in Adults | GH | Daily injection under the skin (very small needle) |
| PRL | None | - |
| Oxytocin | None | - |
| Antidiuretic Hormone (Vasopressin) | Desmopressin | Tablet, once to three times daily; or through a nasal tube or by nasal spray |

What are the Benefits of Hormone Treatment(s)?
SYMPTOMS DEPEND ON WHICH HORMONE(S) ARE MISSING.
The goal of hormone replacement therapy is to enable the patient to live a normal life, feel well, and not have the consequences of hormone deficiency (see Table 2). With proper hormone replacement, this goal can be achieved.
Estrogen replacement is advised for premenopausal women with estrogen deficiency who are at risk of developing osteoporosis and who, according to recent studies, may also have increased cardiovascular risk factors.
Men with hypogonadism or testosterone deficiency due to pituitary disease are at risk for developing osteoporosis and sexual dysfunction. Treatment with testosterone may improve sexual function and strengthen bones. Testosterone has also been shown to increase muscle mass and decrease fat mass.
Although there is no cure for hypopituitarism, it is treatable. Successful hormone replacement therapy can enable a patient to live a normal life, feel well, and not have the consequences of hormone deficiency.
In adults who are GH-deficient, replacement therapy may improve quality of life and body composition (reduces fat mass, improves bone mass). Some studies have shown improvement in measures of cholesterol and improved cardiac function.
Several large studies have reported a slight reduction in life span due to vascular causes (heart attacks, strokes) and infections in patients with long-standing hypopituitarism. The reasons for this are not clear —but could be due to untreated or inadequately treated hormone deficiencies or to ill effects of treatment (particularly radiotherapy).
TABLE 2. SYMPTOMS AND SIGNS OF PITUITARY HORMONE DEFICIENCY
| PITUITARY HORMONE | TARGET ORGANS | TARGET ORGANS |
|---|---|---|
| ACTH | Adrenal glands: cortisol and DHEA | Fatigue, low sodium in blood, weight loss, skin pallor |
| Hypertension | Thyroid gland: thyroid hormone | Fatigue, weight gain, dry skin, sensitivity to cold, constipation |
| TSH | Ovaries: estrogen, progesterone; ovulation | Loss of periods, loss of sex drive, infertility |
| LH and FSH in Women | Testes, testosterone, sperm production | Loss of sex drive, erectile dysfunction, impotence, infertility |
| GH in Children & Adolescents | Bone, muscle, fat | Lack of growth (height); increased body fat, failure to achieve normal peak bone mass |
| GH in Adults | Whole body | Poor quality of life, increased body fat, decreased muscle and bone mass |
| PRL | Breast | Inability to breastfeed |
| Oxytocin | Breast, Uterus | Complete deficiency could make breastfeeding difficult |
| Antidiuretic Hormone (Vasopressin) | Kidney | Frequent urination (day & night), dilute urine, excessive thirst |

What are the Risks of Hormone Treatment(s)?
DOSES HIGHER THAN NEEDED HAVE HARMFUL EFFECTS
Hormone replacement at doses higher than needed, especially in the case of cortisol, may have harmful effects on the heart, bones (osteopenia or osteoporosis), and other organs. In fact, patients on long-term cortisol therapy should have periodic bone density tests. Too much cortisol can increase the risk of infection.
Individuals treated with too low a dose of cortisol run the risk of adrenal insufficiency. All patients must take additional cortisol under stressful situations.
Side effects of hGH replacement include ankle swelling, joint aches, and an increase in blood sugar levels. Treatment with hGH may require increased doses of cortisol in patients with low adrenal function.
An overdose of desmopressin may be dangerous, resulting in water retention and reduced sodium levels in the blood. When the sodium level drops too low, patients may get quite sick and have seizures.
As with the general population, patients with hypopituitarism should be screened for additional cardiovascular risk factors and take steps to control the risk by conventional means: avoid obesity by adopting a healthy lifestyle (don’t smoke, eat a healthy diet and exercise regularly); take blood pressure medication to manage high blood pressure and use lipid-lowering drugs to control high cholesterol levels. Patients should work closely with health care specialists such as endocrinologists, primary care physicians, nurses, and support workers to ensure that each pituitary hormone deficiency is appropriately assessed and, where appropriate, replaced.

Is Life-Long Treatment Necessary, and What Precautions Are Necessary?
USUALLY REQUIRES LIFE-LONG TREATMENT
If the pituitary gland is permanently damaged, proper hormone replacement usually requires life-long treatment. The optimal dose is then considered the “maintenance” dose, and it should become a regular part of daily life.
However, some deficiencies can be transient. For example, after undergoing pituitary surgery, some patients experience temporary hormone deficiencies, which recover over time. DI may also occur for just a few days or weeks after pituitary surgery.
All patients taking cortisol or desmopressin should carry a Steroid Alert or MedicAlert Card with them or wear a MedicAlert bracelet or necklace at all times. These serve to notify attending doctors and health care professionals that the patients have a pituitary hormone deficiency and are taking steroids. All patients taking steroids must increase their daily dose if they become ill or have any condition for which they would normally seek medical advice (e.g., urinary tract or chest infection, severe stress). The nature of the stress dictates the degree of increase necessary. For instance, very severe stress, such as abdominal surgery, requires high daily doses, usually given by injection. Lesser degrees of stress, such as a high fever, might require a doubling of the dose, whereas a cold may require only a small increase or no change in dose. Vomiting and/or severe diarrhea reduces the absorption of oral steroid tablets; in this situation, patients should seek medical attention urgently for intravenous or intramuscular steroids.
Once a patient’s dose has been increased, the patient should remain at the boosted dose until the condition resolves before returning to the usual maintenance dose. Patients should consult their physician before changing their steroid dose.

How is Treatment Followed?
PATIENT'S RESPONSE TO FIND THE RIGHT DOSE
When hormone replacement treatment is first started, it may take time to determine the patient’s response and to find the best dose. Thus, frequent visits with the endocrinologist and repeated blood tests may be needed.
After the optimal hormone dose is determined, a patient should be monitored every six months. Ideally, all patient symptoms should be further evaluated by blood tests. This is particularly important for patients who have received pituitary or whole-brain radiation since the loss of pituitary function may occur at any time.

Is Fertility Possible if I have Hypopituitarism?
FERTILITY MAY BE RESTORED
Fertility is never certain for anyone, even adults with a normal pituitary gland (10% of all “normal” couples are infertile). Infertility related to hypopituitarism is the result of LH and FSH deficiency. Sometimes, PRL levels are high, which results in reduced LH and FSH levels. In such a situation, fertility may be restored by lowering PRL levels with medication such as bromocriptine or cabergoline.
A large pituitary adenoma or hemorrhage can also cause LH and FSH deficiency. In that case, treatment (by injection) of LH and FSH equivalents can stimulate the ovaries to produce eggs or the testes to produce sperm, assuming the ovaries and testes are otherwise normal. The sperm cycle in men is long, over 70 days, and a year or more of treatment may be required for a man to achieve a sperm count adequate to father a baby. Thus, for men who are interested in fertility, it is prudent to obtain a semen analysis at the time a pituitary problem is diagnosed. If the patient has an adequate sperm count at diagnosis, sperm can be collected and frozen for future use. Unfortunately, the current technology for freezing eggs is not yet optimal.
Important: If a woman with hypopituitarism becomes pregnant, she should be monitored closely. Doses of thyroid and steroid replacement may need to be adjusted. GH treatment is not approved for use in pregnant women.

What Do I Need to do if I have a Pituitary Hormone Deficiency?
CAN DEVELOP IN PEOPLE OF ANY AGE
1. Get involved. Undergo necessary tests to determine which pituitary hormone or hormones are deficient and require replacement.
2. Be attentive. When beginning hormone replacement therapy, pay close attention to the effects of treatment and be willing to take blood tests to determine the best dose.
3. Cooperate. Take medication as prescribed and at the correct times; do not take calcium at the same time as thyroid hormone, as it can inhibit absorption from the stomach.
4. Stick with it. Attend regular visits with the endocrinologist to ensure you find the hormone replacement therapy right for you.
5. Follow up. Have appropriate tests (blood tests, magnetic resonance image scans) to determine if there is a recurrence of the pituitary adenoma or other type of growth.

If You Require Hydrocortisone, Prednisone, or Desmopressin Replacement:
WEAR A MEDICAL ALERT BRACELET
1. ALWAYS CARRY A MEDICAL ALERT CARD (STEROID ALERT CARD IN THE UK AND OTHER EUROPEAN COUNTRIES) AND WEAR A MEDICAL ALERT BRACELET OR NECKLACE AT ALL TIMES THAT STATES YOU HAVE THIS CONDITION
2. When you have another illness, such as the flu, pneumonia, or urinary tract infection, increase the dose of hydrocortisone or prednisone during the illness.
If you cannot take the pills, go to an Emergency Department to receive hydrocortisone intravenously.

Summary
CAN DEVELOP IN PEOPLE OF ANY AGE
There is no “cure” for pituitary hormone deficiency. However, similar to patients with high blood pressure, there are effective treatments for these conditions. Thus, it is very important to diagnose hormone deficiencies and determine the optimal dose of hormone replacement. With appropriate treatment taken as directed, individuals with pituitary hormone deficiencies should be able to live normal, productive lives.
PITUITARY DISORDERS MENU